Wide Complex Tachycardia: V Tach or Wide-complex SVT
(C) 2020 – Vernon R Stanley, MD, PhD | Courtney Stanley, PA-C
Taken from the STEMI Review Course (4 Hours Cat I CME/CE)
Wide Complex Tachycardia – Is it Ventricular Tachycardia or Wide-complex SVT?
First, we will review of Supraventricular Tachycardia (SVT) & then Ventricular Tachycardia:
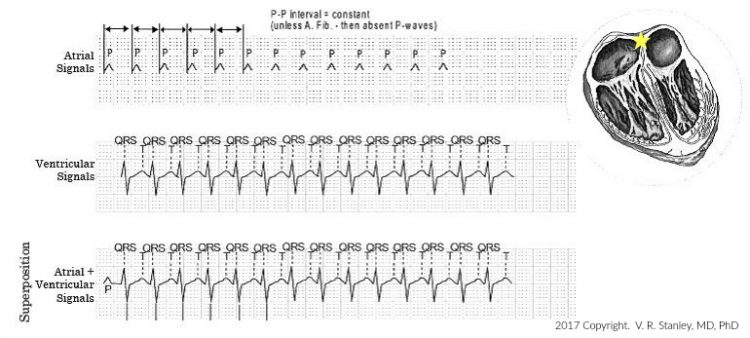
Supraventricular Tachycardia
Spontaneous focus of irritably of Atrium (supraventricular) that discharges at a rapid rate. (Please note that although Atrial Fibrillation on page 28 is supraventricular in origin, the term SVT is typically reserved for regular rhythms (either atrial, with p-wave often hidden, or junctional).
Pearl: Often the P-waves of SVT cannot be discerned (sometimes may appear as a tiny notch), since the rate is so rapid that it blends with the T-wave.
Animated Rhythm of SVT…
Clinical Comment: If clinically indicated, treatment consists of vagal maneuvers and IV Adenosine.
SVT Characterized by:
- Rate = 150-250 bpm
- Rhythm = Regular
- QRS complexes are narrow (unless a conduction defect of LBBB, RBBB or IVCD is present)
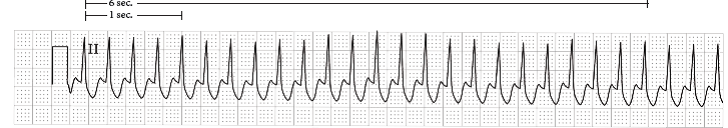
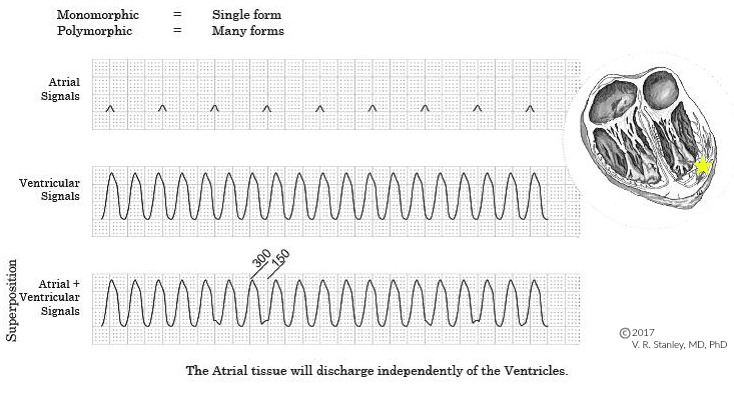
Ventricular Tachycardia (Monomorphic)
Features of V Tach:
- QRS-QRS complexes produce a rhythm that may be slightly irregular.
- QRS duration will be at least 0.12 sec and its shape will often be bizarre
- QRS-T often unable to distinguish QRS from T-wave
- Rate usually 150-250 bpm
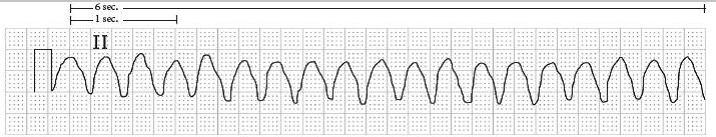
Animated Rhythm of V Tach…
Clinical comment: This is a life-threatening rhythm and must be addressed promptly. It might degenerate to Ventricular Fibrillation and death.
Development Mechanisms of Ventricular Tachycardia
Ventricular Tachycardia occurs via two common mechanisms: increased automaticity and reentry.
(I will discuss these two mechanisms below, primarily for the sake of completeness, and is not intended to represent a thorough discussion of these topics.)
What is most important is the recognition of V Tach and differentiating it from wide complex SVT. It is clearly true that V Tach is a more life threatening rhythm and that the treatment mode is very different from SVT.
- Mechanism 1: Increased automaticity (uncommon) – If an irritable focus of the terminal Purkinje cells discharges at a rapid rate, > 150 bpm, this will produce a QRS complex as discussed previously (wide > 0.12 sec, bizarre-shaped)
- Mechanism 2: Reentry (most common) – Reentry tachycardia can occur from the spontaneous discharge of a terminal Purkinje cell if its subsequent propagation encounters a branch in its pathway:
Branch I – Normally conducted (Antegrade) pathway
Branch II – Refractory pathway (Antegrade signal is blocked)
When the signal traverses Branch I and reaches the distal end, if the distal end of Branch II has adequately repolarized (not refractory), one might suggest that the signal then retrograde propagates up Branch II (this is indeed what happens). At this point, the signal has traveled in a circle and has returned to its starting point.
If the proximal end of Branch I has adequately recovered (repolarize) and is receptive (not refractory), the cycle will repeat itself.
If this cyclic impulse is sustained (3 times or greater) it is labeled ventricular tachycardia. This mechanism of V Tach is called reentry. It is due to a circular conduction (circus).
Now for the focus of this particular topic:
The challenge most often becomes, is this V Tach or is it Wide Complex SVT? Most importantly, the clinical picture is the most important clue but otherwise the following findings are more suggestive of V Tach:
- Look at lead avR for the following:
- Initial R-wave – suggests V Tach
- Initial R-wave or Q-wave width > 1mm – suggests V Tach
- Notching present on the initial downstroke of a predominately negative QRS complex – suggests V Tach
- Ventricular activation-velocity ratio Vi / Vt < 1 – suggests V Tach
where Vi = Voltage deflection at end of initial 40 ms of QRS
where Vt = Voltage deflection at terminal 40 ms of QRS
2. Severe Right Axis Deviation (Lead I negative, Lead avF negative)
3. AV dissociation (if P-wave present, no relationship between P and QRS)
4. Slightly (minimal) irregular rhythm
5. |QRS| > 0.14 sec
6. Lead V1 all upright with taller initial rabbit ear
7. All negative V6
8. Precordial leads V1 to V6 all negative
9. Precordial leads V1 to V6 all positive
10. Capture or fusion beats present
11. Previous old tracing demonstrating QRS complexes of a different morphology than the current tracing
12. Absence of an RS complex in all precordial leads
13. If |R-S| interval > 2.5 mm wide in any one precordial lead where |R-S| is beginning of QRS to low point of S-wave
14. Lead II |R-S| > 1.25 mm – OR – |Q-R| > 1.25 mm
15. If LBBB pattern and |Q-R| > 1.5 mm wide in Leads V1 or V2
16. If RBBB pattern and all positive lead V1
17. If RBBB pattern and rS complex in Lead V6
18. If LBBB pattern and initial R > 1 mm wide Lead V1
19. Notching on the initial downstroke of a predominately negative QRS complex in Lead avR
20. If LBBB pattern and there is a Q or QS in Lead V6
Please note that these findings as stated above are not 100% specific or 100% sensitive, i.e. there are significant numbers of false positives and false negatives, but the more of these clues satisfied in a given tracing, the more likely it is “V Tach”; otherwise the choice is “wide complex SVT”.